テーラーメイド グローレFドライバー
(税込) 送料込み
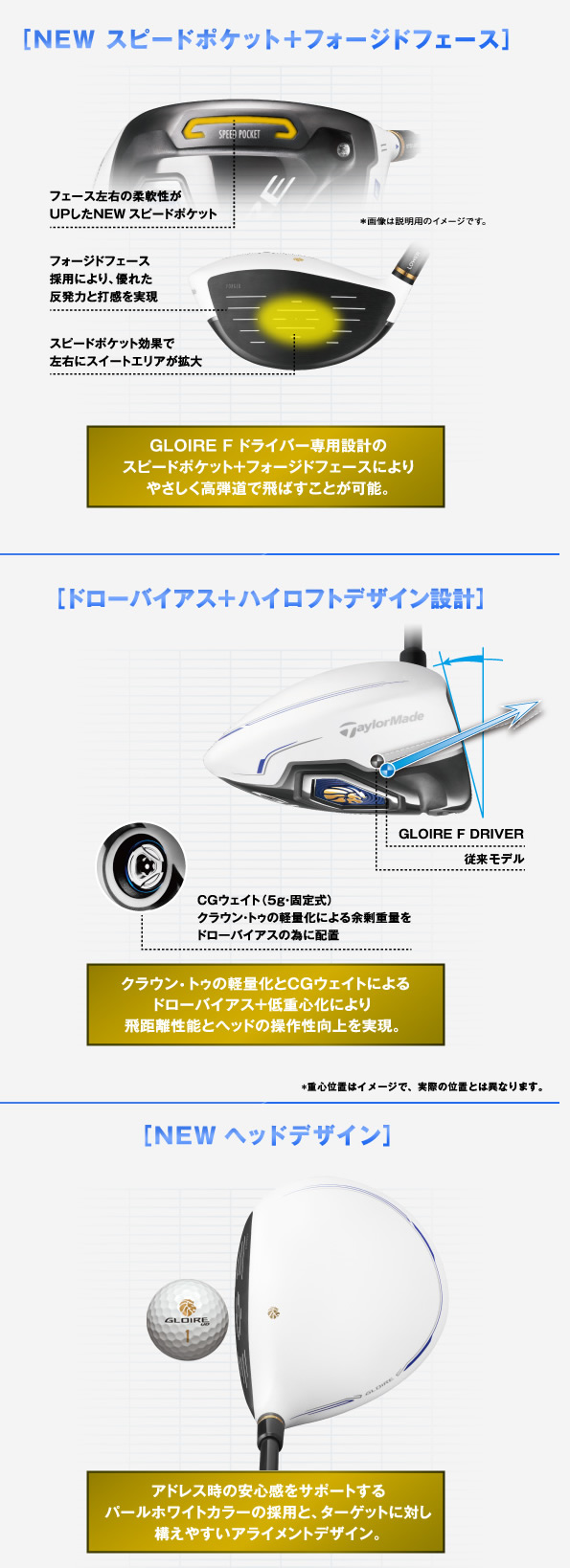
商品の説明
商品説明
ロフト角:9.5°シャフト:マミヤ55ゴールド
フレックス:X
※あまり使用してないので擦り傷も少なく美品です。
3760円テーラーメイド グローレFドライバースポーツ/アウトドアゴルフTAYLOR MADE(テーラーメイド) GLOIRE F ドライバー A3503708 SR 11 46in今が買いどき!高性能で高コスパ!テーラーメイド「グローレF & F2
テーラーメイド グローレ F ドライバー(2014年)(1/5)|マーク金井の
テーラーメイド グローレ F ドライバー - ジーワンゴルフ
TAYLOR MADE(テーラーメイド) GLOIRE F ドライバー A3503708 SR 11 46in
ドライバーNO.1の座は「グローレ F」に決定! - みんなのゴルフ
テーラーメイド グローレ Fドライバー - クラブ
テーラーメイドテーラーメイド グローレF ドライバー - everestgranite.ca
テーラーメイドゴルフ GLOIRE F ドライバー|ゴルフ用品・ゴルフクラブ
TaylorMade Golf - Fairways - GLOIRE F
テーラーメイド グローレFドライバーの+inforsante.fr
Amazon.co.jp: 【中古】テーラーメイド GLOIRE グローレ F ドライバー
グローレFドライバー 11度SR-
新品の通販】 グローレF ドライバー テーラーメイド TaylorMade GROILE
2024人気SALE テーラーメイド グローレf ドライバー QSnqG
テーラーメイド グローレ ドライバー新旧モデル3本打ち比べ!<スッパ
正規取扱店】 【GW特別格安提供】テーラーメイド グローレFドライバー
テーラーメイド グローレFドライバーの+inforsante.fr
普通の人が飛ばすならこれ! GLOIRE F (グローレF)ドライバー(2014
安心の保証付き テーラーメイド グローレFドライバー10度 | www
テーラーメイド グローレ F ドライバー(2014年)の試打レビュー
軍派遣 テーラーメイド グローレF ドライバー R | emplumado.mx
テーラーメイド グローレ F ドライバー - ジーワンゴルフ
ドライバーNO.1の座は「グローレ F」に決定! - みんなのゴルフ
テーラーメイド グローレFドライバー 10゜-
グローレ F(GLOIRE F)ドライバー ヘッド - クラブ
SALE|公式通販| クラブ 【テーラーメイド】 グローレFドライバーヘッド
グローレ F ドライバー-
適当な価格 テーラーメイド グローレ F ドライバー | www.kkkawata.co.jp
今が買いどき!高性能で高コスパ!テーラーメイド「グローレF & F2ドライバー」
テーラーメイド グローレFドライバー 10.5ゴルフ - クラブ
楽天市場】【中古】テーラーメイド GLOIRE F ドライバー 10° S
テーラーメイド グローレFドライバーヘッド単品 ロフト:11度 商品の
GLOIRE(グローレ) F ドライバー 2014 GLOIRE GL-3300 1W 10 S
TaylorMade - テーラーメイド グローレF ドライバーの+urbandrive.co.ke
テーラーメイド グローレ ドライバー新旧モデル3本打ち比べ!<スッパ
TaylorMade テーラーメイド 中古ドライバー GLOIRE F (付属有) 11゜の
希少 黒入荷! アイアン【テーラーメイド グローレF テーラーメイド
50%OFF テーラーメイド GLOIRE F ヘッド単品 ドライバー グローレ
グローレ Fドライバー 11度 ヘッド単品 - クラブ
テーラーメイド グローレF ドライバー - ゴルフ
商品の情報
メルカリ安心への取り組み
お金は事務局に支払われ、評価後に振り込まれます
出品者
スピード発送
この出品者は平均24時間以内に発送しています